What specialist deals with hemorrhoids
Contents:
Hemorrhoids are a chronic condition that can come back if not seen by a doctor. In addition, there are a few complications that can arise if they are not properly treated. The West Valley Colon and Rectal Surgery Center team says that patients can develop what is known as a strangulated hemorrhoid. This means that the hemorrhoid has stopped being supplied blood, and as a result, the tissue can die off and leave the patient in a lot of pain.
Not all hemorrhoids need to be seen by one of our experts, but if topical creams or medications from the pharmacy aisle have not effectively treated your pain, it may be time to come in, especially if you continue to experience rectal bleeding. Our physicians will be happy to provide you with a confidential exam and walk you through the proper course of treatment.
Everything You Need to Know About Hemorrhoids with Dr Michael Valente | Cleveland Clinic
If you have any questions or wish to make an appointment, please call our office at Thank you again for visiting our weekly blog. Over 1 million visits to the doctor in the United States alone every year and that's hemorrhoids. Hemorrhoids are actually part of our normal anatomy. Every single person listening to this podcast has hemorrhoids whether you know it or not.
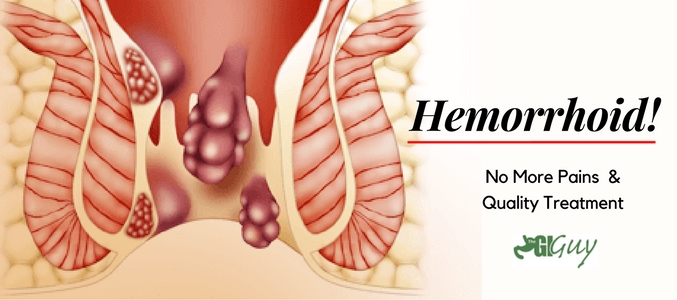
And what type of function do people have that hemorrhoids would be able to do? Hemorrhoids, in their normal resting state, fill with blood and they help actually keep some continence or control of our gas, our bowel movements, under normal circumstances. So I get a lot of people that will go online and they'll have some anal rectum complaints, and one of the very first things that come up is hemorrhoids. And one of the first things that you'll see is external hemorrhoids versus internal hemorrhoids. What's the difference between the two? Internal hemorrhoids are as the name states — inside.
And internal hemorrhoids usually are a cause of rectal bleeding. They can cause pain sometimes if they swell and bulge, or prolapse. External hemorrhoids are usually what we could see from the outside. Those are also referred to as sometimes skin tags, and sometimes external hemorrhoids can be quite painful if they become what we call thrombosed external hemorrhoids.
But one of the things is that patients get them removed. So if they're normal and everybody has them, I don't understand this. Why would somebody need to have their hemorrhoids removed?
Hemorrhoids
When hemorrhoids become problematic or troublesome they, they become what we call hemorrhoidal disease and, and that's when these normal hemorrhoids that do serve a function become abnormal. And what I mean by that is they overfill with blood, or they become lax or loose, and they prolapse or herniate. And really the hemorrhoids at this stage are causing more problems then they're doing good. And what I mean by that is they may bleed, which is one of the most common problems with hemorrhoids that we see. They can cause pain with the prolapse, quite debilitating pain sometimes.
They secrete mucus and they may cause trouble with keeping hygienic down there as well. So when it reaches that point where they become so troublesome, that's when we recommend some sort of intervention. Let's take a step back and we'll go back up to the symptoms that patients go. You mentioned that patients can have bleeding; is the bleeding associated with hemorrhoid any different from other sources of bleeding along the G. Yes and no. Most hemorrhoidal bleeding occurs with bowel movement or during the active defecation, and a lot of times that bleeding is a bright red in nature, and it usually may drip into the toilet, but usually associated with the act of having a bowel movement.
Other causes of gastrointestinal bleeding can be more severe, more volume, if you will, and maybe associate with other conditions that are more serious. Are there some hints that you might say, hey, this is hemorrhoid bleeding versus some more benign disorders that are in the anal rectal region, that you would say this is associated with another diagnosis? When we usually talk about hemorrhoid bleeding, it's what we would call a painless bleeding most often, as opposed to bleeding that occurs with a bowel movement that may cause severe sharp pain that would point us toward something called an anal fissure.
If we're going to talk about the symptoms that patients get, when should they go and see the doctor? When the patient is having rectal bleeding, we do recommend that they do come to see us because it very well may be just hemorrhoids.
Search form
But you need to have a trained professional colorectal surgeon, if you will, or even your family doctor, really investigate that, because even though the hemorrhoids do bleed, and it's a major cause of anal or rectal bleeding, there could be other causes that we must rule out first. So if I go to the doctor, with or without hemorrhoids or suspicion of hemorrhoids, what can I expect at that doctor visit?
And then after a good conversation about maybe leading us towards a diagnosis, a good examination in the office is compulsory.
And what I mean is usually that consists of a rectal examination and sometimes the use of what we call an anoscope, a small device that usually has a light on it to evaluate the most distal part of the rectum and anal canal. Mike, are hemorrhoids cancer or can they turn into cancer? No, hemorrhoids are not cancer. Hemorrhoids do not turn into cancer. Is that common that it be cancer or is it more common that it's going to be hemorrhoids?
It's most common that it's going to be hemorrhoids. But we don't ever want to take any chances. Yeah, absolutely. So what causes hemorrhoids? Many things — multifactorial, we like to say. I tell a lot of my patients sometimes hemorrhoids are just the act of one's ageing process, where the hemorrhoids, themselves, are getting loose, and they tend to have the effects of gravity like other body parts may as well.
We do see hemorrhoids in very young people as well. And I think one of the most common causes of hemorrhoids is a lack of a good diet and exercise. What I mean by that is people who don't have a good dietary intake of fiber tend to be constipated tend to spend a lot of time on the toilet, a lot of times straining on the toilet to get a bowel movement to come out, and those definitely precipitate hemorrhoidal disease. Let's focus in a little bit about treatment or even first prevention of hemorrhoids.
You mentioned fiber, how much fiber is the average Western diet type person taking? Yeah, the average Western diet is extremely low in fiber. And that may be true, but the average American or Western civilized countries maybe get 10 to 15 grams of fiber in the best of circumstances. What we recommend, as the Society of Colorectal Surgeons, is between 25 and 35 grams per day. And the normal western diet really can't achieve that goal, and that's where we get into having supplemental fiber as part of one's daily routine.
There's a lot of supplemental fibers out there, and it's difficult if I'm a patient, I'm looking at this grocery store aisle full of fiber and I'm thinking where do I start?
What do I choose? Where do I go? I recommend, and most of us do, the powdered fiber supplements that tend to work the best. And the key ingredient is what we call psyllium in most of the fiber products. And the question goes back to, will it work right away? It does not. It's a slow gradual process where you need to start with a very low dose and work your way up, and every patient is going to have their kind of sweet spot amount that they need each day or every other day to get the right effect. Because if one takes too much fiber too quickly, the patient will have some side effects of bloating, gas and potentially too much bowel movement.
And we want to avoid that, so we start slow and kind of work our way up. I think it's also important that patients understand that with any fiber product out there you need to make sure you take enough water in there because, for sure, dehydration can cause symptoms. Mike, you said something a little bit earlier about having good bowel habits and good bowel regimens, and that potentially having poor bowel regimens and bowel habits can lead over time to exacerbation of hemorrhoids. What does that mean having good bowel habits?
To remove a hemorrhoid using rubber band ligation, your doctor inserts a small tool called a ligator through a lighted tube scope in the anal canal and grasps the hemorrhoid with forceps. Sliding the ligator's cylinder upward releases rubber bands around the base of the hemorrhoid. Rubber bands cut off the hemorrhoid's blood supply, causing it to wither and drop off. For persistent bleeding or painful hemorrhoids, your doctor may recommend one of the other minimally invasive procedures available.
These treatments can be done in your doctor's office or other outpatient setting and do not usually require anesthesia. Rubber band ligation. Your doctor places one or two tiny rubber bands around the base of an internal hemorrhoid to cut off its circulation.
Butts and Guts, a Cleveland Clinic podcast exploring your digestive and surgical health from end to end. If you don't have celiac disease, the answer can be complicated. Wilkinson JM expert opinion. I tell a lot of my patients sometimes hemorrhoids are just the act of one's ageing process, where the hemorrhoids, themselves, are getting loose, and they tend to have the effects of gravity like other body parts may as well. Depending on your signs and symptoms, your doctor may refer you to one or more specialists — including a doctor with expertise in the digestive system gastroenterologist or a colon and rectal surgeon — for evaluation and treatment. While coagulation has few side effects and may cause little immediate discomfort, it's associated with a higher rate of hemorrhoids coming back recurrence than is the rubber band treatment. Anything my mother makes.
The hemorrhoid withers and falls off within a week. This procedure is effective for many people. Hemorrhoid banding can be uncomfortable and may cause bleeding, which might begin two to four days after the procedure but is rarely severe. Occasionally, more-serious complications can occur. Coagulation infrared, laser or bipolar.
- Hemorrhoids - Gastrointestinal Diseases, Conditions & Treatment;
- Everything You Need to Know About Hemorrhoids with Dr. Michael Valente;
- dell inspiron 15 coupon code.
- Cleveland Clinic Menu.
- 4 Signs Your Hemorrhoids Warrant a Doctor's Visit.
Coagulation techniques use laser or infrared light or heat. They cause small, bleeding, internal hemorrhoids to harden and shrivel.
While coagulation has few side effects and may cause little immediate discomfort, it's associated with a higher rate of hemorrhoids coming back recurrence than is the rubber band treatment. If other procedures haven't been successful or you have large hemorrhoids, your doctor may recommend a surgical procedure.
Your surgery may be done as an outpatient or may require an overnight hospital stay. Hemorrhoid removal. In this procedure, called hemorrhoidectomy, your surgeon removes excessive tissue that causes bleeding.
More Cleveland Clinic Podcasts
Various techniques may be used. The surgery may be done with a local anesthetic combined with sedation, a spinal anesthetic or a general anesthetic. Hemorrhoidectomy is the most effective and complete way to treat severe or recurring hemorrhoids. Complications may include temporary difficulty emptying your bladder and resulting urinary tract infections.
When to see your doctor about your hemorrhoids
Most people experience some pain after the procedure. Medications can relieve your pain. Soaking in a warm bath also may help. Hemorrhoid stapling. This procedure, called stapled hemorrhoidectomy or stapled hemorrhoidopexy, blocks blood flow to hemorrhoidal tissue.
It is typically used only for internal hemorrhoids. Stapling generally involves less pain than hemorrhoidectomy and allows for earlier return to regular activities. Compared with hemorrhoidectomy, however, stapling has been associated with a greater risk of recurrence and rectal prolapse, in which part of the rectum protrudes from the anus. Complications can also include bleeding, urinary retention and pain, as well as, rarely, a life-threatening blood infection sepsis. Talk with your doctor about the best option for you. If you have signs and symptoms of hemorrhoids, make an appointment with your regular doctor.
Depending on your signs and symptoms, your doctor may refer you to one or more specialists — including a doctor with expertise in the digestive system gastroenterologist or a colon and rectal surgeon — for evaluation and treatment. You can help your doctor by being prepared with as much information as possible. Here are some suggestions to help you get ready for your appointment.